One Health in Action: Building Multidisciplinary Bridges for Improved Global Health Security and Pandemic Preparedness

Kenya Validates Groundbreaking Decision-Making Tool for Public Health Emergencies (DMT-PHE)
October 22, 2025
Kenya advances One Health and Pandemic Preparedness with Launch of Rift Valley Fever Contingency Plan and Human Brucellosis Testing Guidelines
November 5, 202530 October 2025
“Pandemic Preparedness and readiness is strengthened by our ability to decide and act together across disciplines, borders, and communities” Dr. Mark Nanyingi
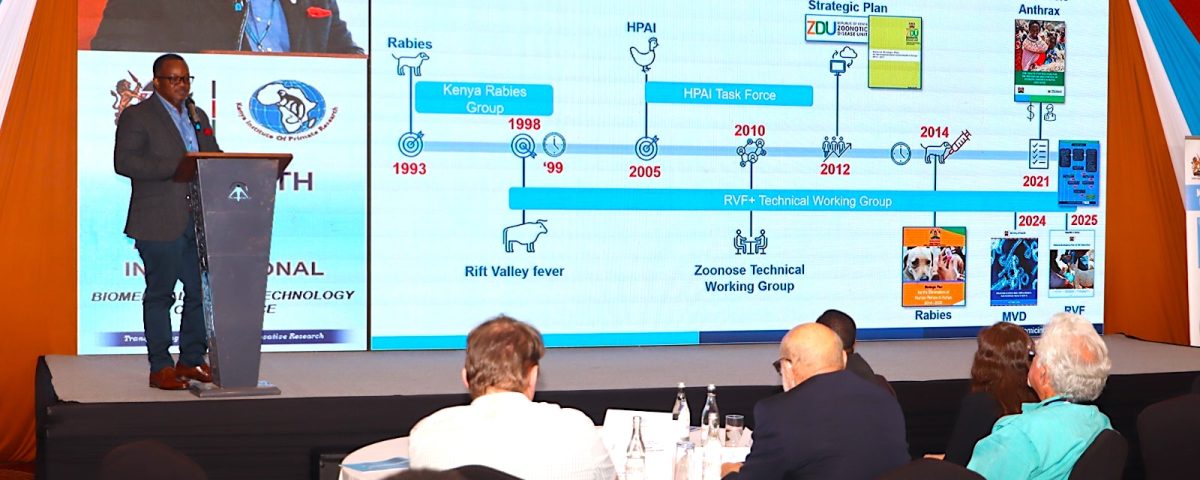
At the 20th International Biotechnology and Biomedical Conference held in Nairobi, under the Emerging and Reemerging Diseases theme, Dr. Mark Nanyingi’s talk of “One Health in Action- Interdisciplinary Approaches in Tackling Public Health Threats” resonated as a rallying call for countries striving to transform global health security from aspiration to action. Kenya’s experience offers a compelling story of how integrated, multisectoral collaboration can move a nation from reactive responses to proactive preparedness in the face of growing public health threats.
Multisectoral mechanisms
Over the past decade, Kenya has built a resilient One Health system that bridges human, animal, and environmental health. The One Health conceptual framework has matured into a functional ecosystem linking national, county, and community institutions. The country’s One Health architecture is anchored on the Zoonotic Diseases Unit that connects the Ministry of Health, the Directorate of Veterinary Services, the State Department of Environment, and the Kenya Wildlife Service through coordinated technical working groups and County One Health Units. ZDU serves as active coordination hub for surveillance, risk assessment, outbreak investigation, and communication across the human-animal and environmental health sectors.
The operational maturity of these systems has been tested in real-world settings. During the 2024 Rift Valley Fever outbreak in Wajir and Marsabit counties, health and veterinary teams collaborated to detect, confirm, and contain infections across both species. The Integrated event-based surveillance (EBS) enabled early signal detection, while both human and animal laboratories provided rapid confirmation that guided evidence based decision making and public health actions embedded in community mechanisms. The recently validated Decision-Making Tool for Public Health Emergencies (DMT-PHE), that was developed by Center for Global Health and Pandemic Intelligence (CGP), has further standardized how outbreak information is escalated and acted upon by different stakeholders. By institutionalizing a clear process for analyzing risk and guiding decisions, Kenya has reduced the time between detection and response—an essential metric for preventing small outbreaks from becoming national emergencies.
Crossborder Coordination and Collaboration
The One Health approach has also expanded beyond borders. Kenya’s collaboration with Ethiopia and Somalia, exemplified through crossborder simulation Exercise COHESION and a tripartite IGAD led communique and memorandum of understanding (MOU), represents a model for regional preparedness. This partnership has improved data sharing, joint surveillance, and synchronized resource mobilization, demonstrating how political commitment and technical alignment can strengthen regional resilience. Equally transformative is the shift at the community level, where pastoralists, traders, and local leaders are recognized as vital contributors to early warning systems. Embedding risk communication and community engagement into all One Health operations ensures that response begins where risk originates at the grassroots.
Digital Health and Artificial Intelligence
Beyond coordination, Kenya’s One Health journey is increasingly defined by science and innovation. Decades of zoonotic research in the Horn of Africa have laid the foundation for a new wave of data-driven surveillance. Artificial intelligence and digital health technologies are now being applied to epidemic forecasting, enabling Kenya to predict climate-sensitive and zoonotic outbreaks with unprecedented precision. Through AI-informed simulation exercises, decision-makers are being trained to interpret predictive data, transforming foresight into policy and action. The integration of data across human, animal, and environmental domains is gradually creating a unified epidemic intelligence ecosystem that embodies the future of health security.
Emerging Challenges and Opportunities
Still, the road ahead is not without challenges. Fragmented governance, workforce gaps, and uneven data-sharing mechanisms continue to limit the full potential of the One Health framework. Financial sustainability remains a persistent concern, as long-term coordination requires dedicated domestic funding and institutional ownership. Meanwhile, external pressures — from Climate variability, Climate Change and land-use change to increased human-animal interactions are expanding the frontiers of infectious diseases risk. Yet, these challenges have also reinforced Kenya’s resolve to innovate, adapt, and strengthen its interconnected systems.
The country’s progress reflects an important dimension:
“Health security is not achieved through isolated interventions, but through relationships, shared knowledge, and mutual accountability across disciplines. It is the product of collaboration between doctors and veterinarians, ecologists and data scientists, policymakers and communities. This interdependence is what makes the One Health approach both necessary and transformative,” Dr. Mark Nanyingi
Kenya’s milestones demonstrate that for successful implementation and operationalization of One Health, there is a need for commitment to unity in the face of complexity. By investing in digital innovation, empowering communities, and embedding collaboration into its health systems, the country is demonstrating that multidisciplinary bridges can hold the weight of global public health threats and pandemics. The journey from fragmented systems to integrated preparedness continues, and with each step, the vision of a safer, healthier world comes closer to reality.